Lung Cancer
.png.aspx)
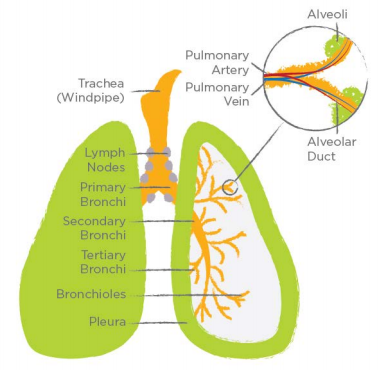
The lungs are a pair of spongy organs in the chest and are separated from each other by the heart. The lungs are divided into lobes. The right lung has an upper, a middle, and a lower lobe; and the left lung only has upper and lower lobes.
When you breathe in, air flows past your nose and larynx (or voice box) and into the trachea (or windpipe). Just before it reaches the lungs, the trachea divides into two smaller airways called the bronchi, one bronchus for each lung. These airways divide further and further into smaller tubes called bronchioles, which end in the alveoli. The alveoli are microscopic air sacs where oxygen from inhaled air enters the blood; and carbon dioxide leaves the blood and is eventually exhaled.
Each lung is enclosed and protected by the pleura—two layers of thin pleural membrane. The pleural space between these two layers contains a small amount of pleural fluid to lubricate the membranes so they can slide easily over each other when you breathe. Below the lungs is the diaphragm, a thin sheet of muscle that helps you breathe.
Lung Anatomy
Lung Cancer
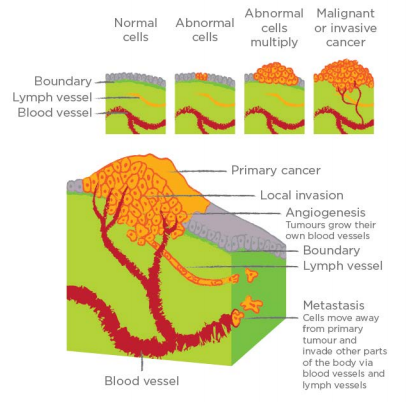
Cells are the building blocks that make up the tissues and organs. Normally, before a cell dies, it makes a new cell to take its place. However, sometimes a cell becomes abnormal and makes many copies of itself. These copies pile up and form a tumour, a lump of abnormal cells. They mimic healthy cells in the body to evade the body’s natural defences.
Benign tumours, like moles and warts, cannot invade their surrounding tissue or spread to other locations in the body.
Malignant tumours are cancerous. They continue to grow and invade the surrounding tissue. Sometimes cancer cells break away from the tumour and travel to other organs via blood or lymph vessels. This process is called metastasis. Cancer can metastasize to any part of the body; however, cancerous cells from a lung tumour commonly spread to the other lung, lymph nodes, adrenal glands (which are located on top of each kidney), bones, brain, and liver.
Cancers are named after the site in which they first develop—in the case of lung cancer, the primary tumour is in the lung. Even when lung cancer spreads to other parts of the body, the diagnosis remains lung cancer; and the cancer that has spread is called a secondary tumour or metastatic lung cancer. Similarly, if cancer from elsewhere spreads to the lungs, it is not referred to as lung cancer, but as lung metastases from the primary site.
Cancer Growth and Metastasis
Lymph nodes are small, bean-shaped structures located throughout your body that are part of the lymphatic system. The lymphatic system is a network of organs, vessels, and lymph nodes that helps circulate body fluids, and defends the body against microbes and abnormal cells.
When there is an infection, injury, or cancer in a part of the body, the lymph nodes in that area get bigger. For example, when you have a cold or a sore throat, the lymph nodes in your neck get swollen. If you visited a doctor with these symptoms, they may have felt your neck to check for these enlarged lymph nodes.
Cancer cells from a malignant tumour will sometimes break away and travel through blood or lymph vessels. The cancer cells can lodge themselves in nearby lymph nodes, which normally filter out microbes and abnormal cells. There, they will grow and divide to form a new tumour, which may shed more cancerous cells that can then spread further in the body.
The spread of cancer to the lymph nodes is an important factor in determining the extent or stage of that cancer. The number of affected lymph nodes, the amount of cancer in them, and how far they are from the primary tumour are all considered when your doctor creates your treatment plan.
The two most common types of lung cancer are non–small cell lung cancer and small cell lung cancer. The words small and non–small refer to the size of the cells found in the tumour and not the size of the tumour itself.
Non–small cell lung cancer (NSCLC) is the most common type of lung cancer— around 80% to 85% of all cases. There are three main subtypes of NSCLC.
-
Adenocarcinoma usually starts in mucus-producing glands and is often found in the outer edges of the lungs. It is the most common form of lung cancer in general, as well as in women and non-smokers. Adenocarcinomas may result from known genetic changes that can be treated with targeted therapy.
-
Squamous cell carcinoma (SCC) usually develops in cells lining the bronchi and larger bronchioles, and is often found in the central areas of the lung. SCC is quite common in smokers. Men are more likely to develop squamous cell carcinoma than women.
-
Large cell carcinoma (LCC) can occur anywhere in the lungs but is usually found near the surface and outer edges of the lungs. LCC is the fastest growing subtype of NSCLC and may grow to a very large size before causing any symptoms.
Adenocarcinoma and LCC are often referred to as non-squamous lung cancer or non-squamous NSCLC.
Small cell lung cancer (SCLC) accounts for about 15% of all lung cancers. These cancers usually develop near the centre of the lungs in the bronchi, and invade nearby tissues and lymph nodes. SCLC is also referred to as oat cell carcinoma because the cancer cells look flat under a microscope.
SCLC behaves quite differently from NSCLC and is more aggressive. The cancer cells divide more rapidly to form large tumours that can spread throughout the body before being detected.
Other types of cancer affecting the lungs
Soft-tissue sarcomas in the lung are rare occurrences. They usually develop in the pleural membranes and grow very slowly.
Carcinoid tumours in the lung are rare, slow-growing tumours that arise from hormone-producing cells in the lining of the bronchi and bronchioles.
Pleural mesothelioma is a rare type of cancer that starts in the pleural membranes that envelope each lung. It is usually caused by exposure to asbestos. Although technically not a type of lung cancer, pleural mesothelioma is treated by the same specialists who treat lung cancer.
For more information on the other types of lung cancer, refer to:
The Demographics of Lung Cancer
Incidence Rates1
-
The incidence rate for lung cancer is higher for males than females, although sex specific rates among younger adults appear to be converging
-
In males, the rising incidence rate of lung cancer began to level off in the mid-1980s and has been declining since then
-
Among females, the rate continued to rise and did not level off until 2006
-
The differences in incidence rates between males and females reflect past differences in tobacco use (in females the drop in smoking occurred approximately 20 years later than it did in males, suggesting that lung cancer incidence rates in females may also begin to decrease in the coming years)
Lung cancer stage1
-
The distribution of stage I lung cancers appeared higher in females (23.7%) than males (17.8%), and the distribution of stage IV lung cancers appeared higher in males (52%) than females (47.1%), but these differences may not be statistically significant
-
There was no obvious pattern in the percent distribution across age groups, except that the percentage of cases where the stage was unknown increased as age increased, from a low of 1.1% among people aged 18–59 years at diagnosis, to a high of 8.8% among people aged 90 years and older at diagnosis.
-
The highest ASIR of stage IV NSCLC was observed for Nova Scotia (38.5 per 100,000) and the lowest in Ontario (25.5 per 100,000). For stage IV SCLC, the highest ASIR was also observed in Nova Scotia (9.0 per 100,000) but the lowest was observed in British Colombia (4.3 per 100,000)
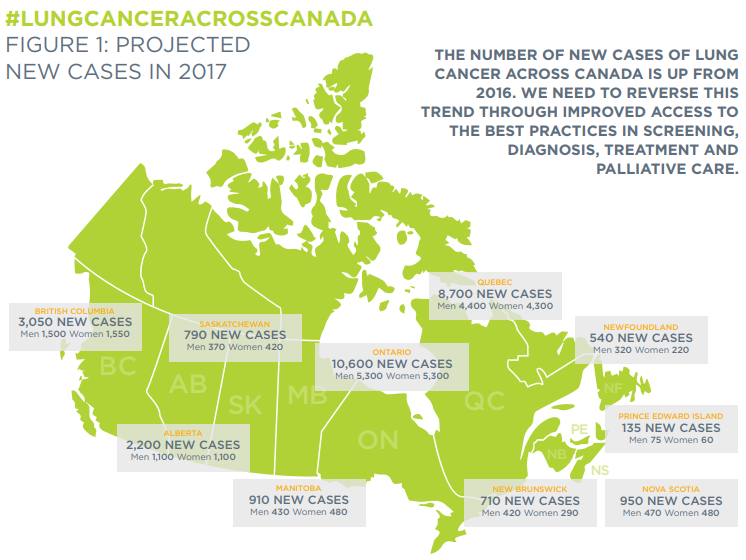
Projected New Cases in 20172
References
1 Canadian Cancer Statistics Advisory Committee. Canadian Cancer Statistics 2018. Toronto, ON: Canadian Cancer Society; 2018. Available at: cancer.ca/Canadian-Cancer-Statistics-2018-EN
2 Canadian Cancer Society’s Advisory Committee on Cancer Statistics. Canadian Cancer Statistics 2017. Toronto, ON: Canadian Cancer Society; 2017. Available at: cancer.ca/Canadian-CancerStatistics-2017-EN.pdf