Research
.png.aspx) Lung Cancer Research Investment
Lung Cancer Research Investment
Canada has been a major contributor on the global scale to advancing the lung cancer fight. Researchers at Canadian hospitals are breaking new ground in developing lung cancer screening programs, enhanced testing and diagnosis. Internationally renowned clinicians advancing treatment possibilities in clinical trials call Canada home. These trials are important to Canadian patients who are being given new opportunities to fight this devastating disease, and then help lung cancer patients globally. New models of patient-care are being pioneered in Canadian clinics and hospitals to improve the experience and standards in lung cancer care all over the world. Ongoing study and evaluation provide patients with a chance at improved outcomes that can benefit Canadians and beyond. Canadian achievements have impacted all corners of the earth.
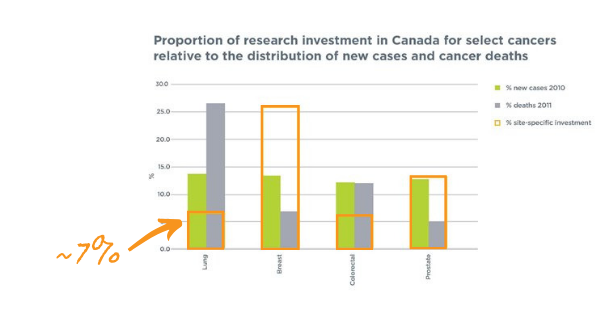
Yet, although lung cancer has the highest mortality of all cancers in Canada, there is a disproportionate amount of research investment allocated to it when compared to other cancers. Advancements are handicapped by vastly inadequate research funding, with only 7% of funding going into lung cancer. In addition, lung cancer only gets 0.1% of cancer donations1.
While it is important that these cancers continue to receive research funding, it is also important to acknowledge the obvious need for additional investment in lung cancer research that, at the very least, matches the significant burden of this disease.
Despite being such a misunderstood and underfunded cancer, there have been many partnerships and milestones to celebrate. Canadian researchers are part of exciting advances, including targeted drug therapies. Latest data suggests that both quality of life and longevity are improving with these new treatments. Other steps forward include the development of high-precision radiation, robotic surgery, other minimally invasive surgery techniques, and recent evidence supporting low-dose CT scans as an effective screening tool for the disease. Each of these advances offers hope. For Canadians fighting a lung cancer diagnosis, it is often hope that spurs their strength to fight another day. It is also hope that drives so many important initiatives for the future.
Treatment Advances
New Treatment Horizons
Dr Rosalyn Juergens, Chair, Medical Advisory Committee, Lung Cancer Canada
Going back just 10 years, there were a limited number of options for treating non-small cell lung cancer (NSCLC). For the vast majority of patients, the treatment options started with chemotherapy combinations followed by more chemotherapy if the first line of treatment failed. Only a small minority of patients could get personalized treatments. Today, however, due to major advances, the treatment landscape has changed. Immunotherapy is now a potential treatment for the majority of patients with lung cancer and we have more patients on targeted therapy. Even those patients who were on targeted therapy a few years ago now have more options available. Unlike years ago, we can now prioritize a patient’s treatment journey to offer the best treatment as early as possible. Although statistics from the Canadian Cancer Society continue to show disappointing survival metrics with the diagnosis of lung cancer, improvements will become evident in the upcoming years. While it is fantastic that we are expanding the amount of time people are living with lung cancer, it is also equally important to ensure patients have a good quality of life while receiving those treatments. New treatments recently approved have shown improvements in patient’s quality of life as well as survival compared to the standard comparators. Better treatment quantity and quality are fortunately going hand in hand. Some of the most excitement in 2018 was generated through advancements in the management of stage III non-small cell lung cancer. With the addition of immunotherapy consolidation to standard chemotherapy and radiation, we already know we are extending lives. We hope that further follow up data will show that we are truly curing more of these patients. Also gaining momentum are early screening programs, as seen with the pilot programs in Ontario. If physicians can diagnose patients at stage I versus stage IV, the chances of patients living longer is vastly improved and the probability of being cured is higher. Reflecting on the NELSON Study presented at the 2018 IASLC World Conference for Lung Cancer, with such screening programs in place for high risk patients, more cases are diagnosed in early stages when surgery is often an option. Screening also shifts the pendulum by diagnosing patients earlier, leaving fewer cases diagnosed in advanced and incurable stages. Additionally, we also cannot underscore the importance of smoking cessation and smoking avoidance. It is important for screening programs to go hand in hand with smoking cessation programs. Everyone with lungs needs to be mindful of exposures and keeping optimal lung health! My hope for the future of lung cancer is a world where medical oncologists, like me, are out of business. We need to identify an optimal way to screen. While the current screening method is through CT scanning in high-risk populations, I hope patients in the future can be screened through other means such as blood or breath tests through which we can discern patients at risk for future lung cancer. I hope that there will come a day when physicians can diagnose all patients at an early stage when a localized approach can result in a cure. Until then, understanding the tumor to personalize treatment options is critically important. Comprehensive and timely genetic profiling allows patients to move forward with the optimal treatment as the first choice. In Canada, health care access is largely universal, but it is also a patchwork quilt in terms of provincial access. I hope for equity across the provinces because, depending on where you live, access to advances or new treatments may be limited. The waiting time for access to new drugs could be time many lung cancer patients do not have. With the support of Lung Cancer Canada we will continue to strive to attain the same opportunity to access approved treatments across the country so lung cancer patients can live longer with a better quality of life.
Game Changing Advancements
Dr. Zhaolin Xu, Professor, Department of Pathology, Faculty of Medicine at Dalhousie University
Advanced testing and diagnostics are revolutionizing treatment pathways in lung cancer like never imagined. New techniques in biomarker tests are identifying specific gene mutations at remarkable speeds, allowing treatment to be highly targeted to an individual patient. With a majority of lung cancer diagnosed at later stages, time means a patient has a better chance of survival, which means everything. Canada has long been a pioneer and leader when it comes to molecular research, challenging the status quo to identify new diagnostic approaches. Dr Zhaolin Xu, Professor, Department of Pathology, Faculty of Medicine at Dalhousie University is studying gene mutations in human lung cancer in addition to pathological assessment of the tumour. New testing techniques now allow patients to be divided into various subgroups based on not only tumour morphology but also molecular profiling, allowing them to receive personalized targeted therapy. In 2005, Dr Xu and his colleagues established the QE II Lung Tumor Bank for research, which is certified by the Canadian Tumor Repository Network (CTRNet). The tumour bank has become one of the largest in the country, a major achievement in Canadian research. “This is a very exciting time in the area of genetic testing for lung cancer, research has become so advanced that it is really giving us a great deal of hope and optimism,” says Dr Xu. “PD-L1 is something that we will start to hear a lot more about, similar to the excitement about EGFR tests a few years ago, I think this will make a dramatic impact in patient survival in the coming years.” According to new research led by Dr Xu, all patients with advanced NSCLC should be tested for PD-L1 at diagnosis. Immune checkpoint inhibitors are fulfilling their promise for the therapy of lung cancer. The expression of immune checkpoint proteins is one mechanism for tumours to deactivate the normal host immune response and evade destruction2. Immune checkpoint inhibitors are efficacious in lung cancer and are targeted against a number of molecular targets. These include the inhibitory programmed death 1 (PD-1) receptor expressed on T cells, natural killer cells, and some B cells2. The two PD-1 ligands are programmed death receptor ligand 1 (PD-L1) and PD-L2, both of which are expressed in a wide range of effector cells, antigen-presenting cells, and T cells2. Dr Xu comments, “This is complex science and we are navigating our way through, making note of the successes and failures to advance our understanding. The Canadian PD-L1 22C3 Quality Validation Project is currently taking place in more than a dozen sites across Canada, with the purpose of standardizing a non-kit based assay for PD-L1 expression. This kind of research can be a game-changer.” Nivolumab and pembrolizumab are two anti-PD-1 antibodies that are approved after failure of conventional chemotherapy for advanced NSLC in Canada. Nivolumab can be prescribed without biomarker testing for PD-L1 expression. Pembrolizumab is limited to patients with PD-L1-positive tumours. Pembrolizumab has also shown improved efficacy compared with platinum doublet in patients who are treatment-naïve with tumours expressing PD-L1 in 50% of tumour cells or more and is approved by Health Canada2. The Expert Committee of thoracic oncology experts feels that PD-L1 testing should be readily available at the time of diagnosis of both non-squamous and squamous NSCLC to allow for rapid initiation of pembrolizumab to eligible patients3. Health Canada approved pembrolizumab in the first-line setting in advanced NSCLC.
Advancements in screening and diagnosis
Dr Stephen Lam MD, FRCPC Chair, Lung Tumor Group & Judah Leon Blackmore Chair, BC Cancer Agency Professor of Medicine University of British Columbia
Canada continues to be an important contributor to the global base of lung cancer research and breaking new ground in the area of screening and diagnostics. Dr Stephen Lam MD, FRCPC Chair, Lung Tumor Group & Judah Leon Blackmore Chair, BC Cancer Agency Professor of Medicine University of British Columbia led a Canadian team who showed that a risk prediction tool to detect early stage lung cancer in high-risk individuals is superior in terms of accuracy compared to other models. The Pan Can Lung Cancer Risk Prediction Model is used to determine if a person should undergo annual computed tomography (CT) screening to detect early-stage lung cancer. The new approach outperformed current screening inclusion criteria such as The US Preventive Services Task Force recommendation. Currently, both the U.S. and Canadian lung cancer screening guidelines are based on age and smoking history. But the Pan Can Model also looks at numerous additional variables such as sex, family history of lung cancer, chronic obstructive pulmonary disease, educational level, and body mass index. In lung cancer, early detection is everything. If a high-risk individual is diagnosed before the onset of symptoms when the cancer is in an early stage, the chances of survival are very good. Dr Lam estimates that up to 75% of patients diagnosed with advanced lung cancer are incurable, but this ratio can be reversed. With the proper screening protocols in place the odds dramatically shift and 75% of the diagnoses are at an early stage when curative treatment is possible. After the Canadian Task Force on Preventive Health Care released a guideline recommending annual lung cancer screening in high-risk adults ages 55-74 who had smoked at least 30 pack-years (e.g. one pack a day for 30 years). British Columbia, Alberta and Ontario were the first to pilot screening programs that will help to shape a provincial standard. Ontario has three sites and the program is expanding to additional sites. British Columbia’s pilot is linked to an international lung screening trial with Australia and Hong Kong to test the use of computer technology as an aide to reading CT scans as well as examining additional lung cancer risk factors such as air pollution and genetic susceptibility to improve the screening selection criteria further. New programs are underway in Montreal and the Alberta pilot has applied for an extension after completion of the pilot. “All of the provinces must move ahead together to implement a standardized screening program. The pilots were good to identify potential issues, but it is time to roll out routine screening like we see in colorectal and breast cancers.” Dr Lam points to the fact that these programs are not expensive and they present dramatic cost savings to the health system. When cancers are detected early, the cure rate improves and we eliminate the costs of treating at a late stage, which is the more expensive stage. Artificial intelligence is starting to become more common in the lung cancer screening discussion. “This is the future,” says Dr Lam. “Artificial intelligence to read CT scans that can accurately detect lung nodules and other changes in the lung, to determine an individual’s risk for lung cancer is where the next innovation in screening will come”. Presented at the World Lung Conference in Toronto in fall of 2018, the Dutch-Belgium NELSON-trial, which is a population-based randomized control trial comparing CT screening with no screening in ever smokers between the age of 50 to 74 years who have smoked at least 15 cigarettes a day for 25 years or more or at least 10 cigarettes a day for 30 years or more and have smoked within 10 years. Between 2004 and 2006, the study enrolled 15,822 participants. The CT screening received a baseline CT and three additional screenings at intervals of 1, 2 and 2.5 years. Analysis at 10 years of follow-up showed a significant 26% reduction in lung cancer mortality in men and up to 61% reduction in mortality in women compared to the no screening group. With two global, large randomized trials demonstrating significant mortality reduction, we now have clear evidence to support the implementation of lung cancer screening similar to breast and colorectal screening that save the lives of countless individuals.
To see what additional research is being done in the fight against lung cancer, visit:
References
1 Thomson, Greg, and Karen Young. "Cancer in Canada." Charity Intelligence Canada, 2011.
2 Kerr KM, Nicolson MC. Non-small cell lung cancer, PD-L1, and the pathologist. Arch Pathol Lab Med. 2016;140:249–54. doi: 10.5858/arpa.2015-0303-SA.
3 Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N Engl J Med. 2016;375:1823–33. doi: 10.1056/NEJMoa1606774